The Challenge
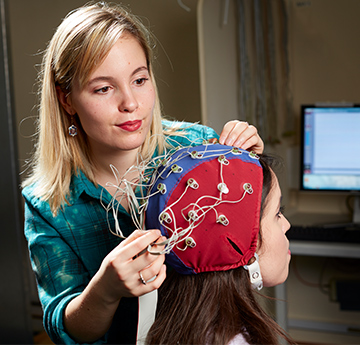
More than 1.3 million people in the UK are living with the long-term effects of acquired brain injury (ABI), affecting one family in every 300 and costing the UK economy around £15 billion per year; around 10% of the annual NHS budget. ABI refers to any injury to the brain which has occurred since birth, such as the result of a road traffic accident, fall or stroke, and it can result in a complex pattern of disability consisting of changes in cognition, mood, and behaviour. The term ‘neurobehavioural disability’ (NBD) is used to capture the range of disabilities that often result in wholesale changes to a person’s character or personality after ABI, with the presence of NBD associated with reduced quality of life, social handicap, and poorer rehabilitation outcomes.
Consequently, making sure that health professionals have the means to reliably detect specific features of NBD from the early stages of recovery, when support is most readily available, and to guide clinical decision-making and treatment throughout the course of rehabilitation, is vitally important.
The Method
Despite the substantial impact a brain injury has on the person, their family, and wider society, detecting the presence of neurobehavioural disability after an acquired brain injury has proved challenging for medical and health professionals. In part, this is because they have not had access to reliable assessment tools to help.
For example, a review conducted by the Swansea University based research team found that many existing NBD tools were unfit for purpose. They were often based on subjective impressions rather than objective observations, were not aligned to cotemporary models of rehabilitation, and some were not originally designed with the symptoms of NBD in mind or for people with ABI.
Consequently, the aim of this research was to fill this significant gap and clinical need by developing a new and reliable NBD tool – The St Andrew’s – Swansea Neurobehavioural Outcome Scale.
As an initial starting point, potential items for the new tool were developed based on the World Health Organisation International Classification of Functioning, Disability and Health framework. Items were then further refined through interviews with relatives of ABI survivors, before a multidisciplinary set of professionals rated ABI survivors on the refined item set.
Rigorous statistical analyses were then applied, showing that the new tool could distinguish between individuals with or without ABI, reliably identify and monitor the presence of NBD over time, and provide a unique basis for treatment planning and evaluation. Subsequent work has also added a supplementary scoring system to the tool to convey the impact of support received on ratings of NBD, further supporting patient care and clinical decision making.